NYACP Board Review Question of the Week
Every other Tuesday, NYACP members are sent a Board Review Question from ACP's MKSAP 18 to test professional knowledge and help prepare for the exam. Participant totals and answer percentages are distributed on the first Thursday of the month in IM Connected, the Chapter's eNewsletter, and are also published on this page.
If you are interested in receiving these questions bi-weekly, join us as a member!
If you are a member who needs to receive the questions and newsletter via email, let us know!
February 24th, 2026
MKSAP 19 Cardiovascular Medicine, Question 58
A 74-year-old man is evaluated in the hospital for a 6-month history of progressive fatigue and exertional dyspnea, along with increasing peripheral edema and abdominal girth over the past 3 months. He also has coronary artery disease, for which he had a coronary artery bypass graft at age 62 years. Medications are metoprolol, low-dose aspirin, and atorvastatin.
On physical examination, vital signs are normal. Jugular venous distention with prominent waveforms is noted. There is no discernable fall in the central venous pressure during inspiration. An early diastolic sound is present. The liver is enlarged and pulsatile. Ascites is present, and peripheral edema extends to the knees bilaterally.
On chest radiograph, sternotomy wires and vascular clips are seen, and small bilateral pleural effusions are present.
Which of the following is the most likely diagnosis?
A. Cardiac tamponade
B. Chronic liver disease
C. Constrictive pericarditis
D. Restrictive cardiomyopathy
Responses Received from Members (503 Responses):
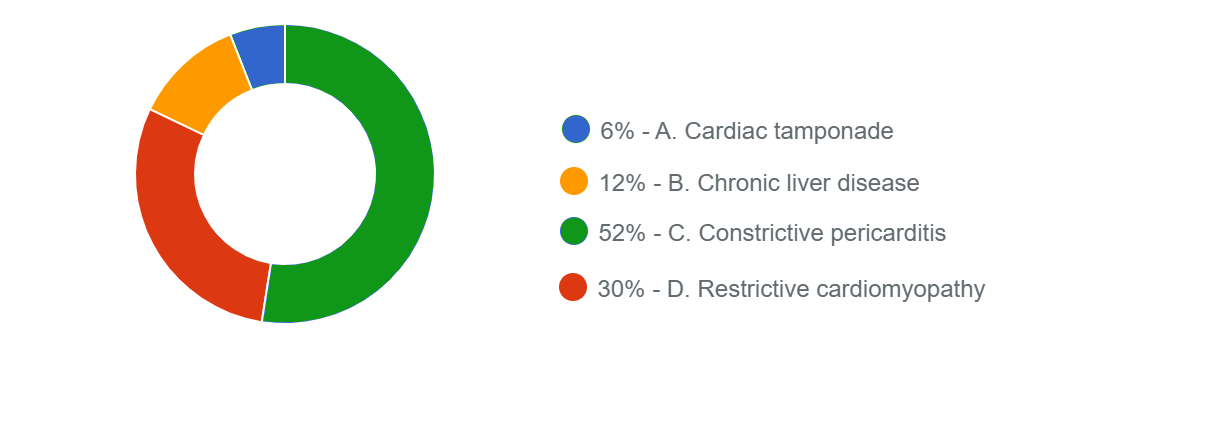
The Correct Answer is: C. Constrictive pericarditis
Educational Objective: Diagnose constrictive pericarditis.
The diagnostic findings are consistent with constrictive pericarditis (Option C), which typically presents with indolent, progressive signs and symptoms of right heart failure, including fatigue and exertional dyspnea. On physical examination, the central venous pressure is elevated in nearly all patients, with prominent x and y descents. The height of the waveform does not fall or may increase during inspiration (Kussmaul sign), reflecting the fixed diastolic volume of the right heart. Early diastolic filling is unimpaired or even accentuated and is followed by sudden cessation when total acceptable volume is met, resulting in a high-frequency early diastolic sound (pericardial knock, heard in <50% of patients). Pulsus paradoxus is less frequent (<20% of patients) in constrictive pericarditis than in cardiac tamponade. Peripheral edema, ascites, hepatomegaly, and pleural effusions are common. Diagnosis of constrictive pericarditis is made with imaging studies and hemodynamic evaluation. Transthoracic echocardiography reveals normal right and left ventricular size and systolic function despite prominent symptoms and findings suggestive of heart failure. Dilatation of the inferior vena cava reflects elevated right-sided filling (right atrial) pressure. Doppler echocardiography and tissue Doppler velocity are required to differentiate constrictive pericarditis from restrictive cardiomyopathy. Although an underlying cause of constrictive pericarditis is not always identified, previous pericarditis, cardiac surgery, chest irradiation, connective tissue disorders, and uremia are common precipitants.
Cardiac tamponade (Option A) can easily be confused with constrictive pericarditis. However, cardiac tamponade is typically associated with pulsus paradoxus and not associated with Kussmaul sign.
A not uncommon misdiagnosis in patients with constrictive pericarditis is cirrhosis. Like patients with constrictive pericarditis, those with cirrhosis may have a palpable liver, ascites, pleural effusions, and peripheral edema. Patients with chronic liver disease (Option B) do not have jugular venous distention, Kussmaul sign, or a pericardial knock, as detected in this patient.
In most cases, clinically differentiating restrictive cardiomyopathy (Option D) from constrictive pericarditis is impossible. Restrictive cardiomyopathy is more likely in a patient with a predisposing systemic disease, such as diabetes mellitus or amyloidosis. In this case, constrictive pericarditis is suggested by the previous coronary artery bypass surgery. Restrictive cardiomyopathy is not associated with a pericardial knock, but this finding is sometimes difficult to distinguish from an S3.
Key Point
- Kussmaul sign and pericardial knock, if present, are helpful clues to the presence of constrictive pericarditis.
Bibliography
Geske JB, Anavekar NS, Nishimura RA, et al. Differentiation of constriction and restriction: complex cardiovascular hemodynamics. J Am Coll Cardiol. 2016;68:2329-47. PMID:
27884252 doi:10.1016/j.jacc.2016.08.
Multiple-choice questions reprinted with permission from the American College of Physicians.
MKSAP 19. © Copyright 2021 American College of Physicians.
ACP MKSAP. © Copyright 2025 American College of Physicians. All Rights Reserved All Rights Reserved.
February 10th, 2026
MKSAP 19 Endocrinology & Metabolism, Question 2
A 46-year-old woman is evaluated for type 2 diabetes mellitus. At the time of her diagnosis 1 year ago, metformin was initiated. Since then, she has been diagnosed with hypertension and dyslipidemia. Medications are metformin, lisinopril, and atorvastatin.
On physical examination, vital signs are within normal limits. BMI is 32. The remainder of the examination is unremarkable.
Today, her hemoglobin A1c measurement is 8.0%.
Which of the following is the appropriate treatment to start next?
A. Dulaglutide
B. Glipizide
C. Insulin
D. Pioglitazone
Responses Received from Members (712 Responses):
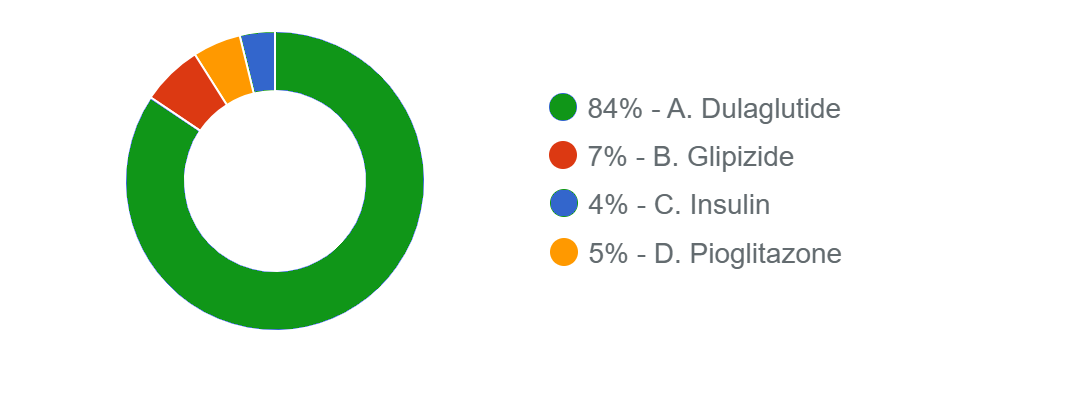
The Correct Answer is: A. Dulaglutide
Educational Objective: Treat type 2 diabetes mellitus in a patient with atherosclerotic cardiovascular disease risk factors.
The best treatment option for this patient is to add dulaglutide (Option A). At the time of diagnosis, metformin was initiated, which is a first-line pharmacologic therapy for the glucose-centric management of type 2 diabetes mellitus. However, her glycemic target is still not at goal. In young, otherwise healthy patients, the American Diabetes Association recommends a hemoglobin A1c target of less than 7% in most nonpregnant adults. Patients should be re-evaluated at 3-month intervals and treatment escalated with additional agents if the hemoglobin A1c remains above goal. In patients with type 2 diabetes mellitus and established atherosclerotic cardiovascular disease (ASCVD) or multiple risk factors for ASCVD, a glucagon-like peptide 1 receptor agonist (GLP-1 RA) or sodium-glucose cotransporter 2 (SGLT2) inhibitor with demonstrated cardiovascular benefit is recommended to reduce the risk for major adverse cardiovascular events, independent of hemoglobin A1c lowering.
This patient has multiple risk factors for ASCVD (hypertension, dyslipidemia, obesity). In addition, GLP-1 RAs are associated with weight loss, which would be beneficial for this patient with obesity. Dulaglutide is a GLP-1 RA with proven cardiovascular benefit.
Glipizide (Option B) is a sulfonylurea and stimulates insulin secretion. It is associated with weight gain and has no ASCVD benefits.
In most patients who need the greater glucose-lowering effect of an injectable medication, GLP-1 RAs are preferred to insulin (Option C). Insulin administration is not associated with the ASCVD benefits of a GLP-1 RA and may also cause weight gain.
Pioglitazone (Option D), a thiazolidinedione, increases peripheral uptake of glucose. Although pioglitazone can possibly decrease cardiovascular disease events, it is associated with weight gain, which is undesirable in this patient with obesity.
Key Point
- In young, otherwise healthy patients, the American Diabetes Association recommends a hemoglobin A1c target of less than 7% in most nonpregnant adults.
- A glucagon-like peptide 1 receptor agonist or sodium-glucose cotransporter 2 inhibitor with demonstrated cardiovascular benefit is recommended in patients with type 2 diabetes and established atherosclerotic cardiovascular disease (ASCVD) or multiple risk factors for ASCVD to reduce the risk for major adverse cardiovascular events.
Bibliography
ElSayed NA, Aleppo G, Aroda VR, et al. 10. Cardiovascular disease and risk management: standards of care in diabetes—2023. Diabetes Care. 2023;46:S158-S190. PMID: 36507632 doi:10.2337/dc23-S010
Multiple-choice questions reprinted with permission from the American College of Physicians.
MKSAP 19. © Copyright 2025 American College of Physicians.
All Rights Reserved.
